Exeter Collaboration for Academic Primary Care (APEx) Blog
Exeter Collaboration for Academic Primary Care (APEx) Blog
Posted by ma403
11 March 2025Written by Dr Luke Mounce

From the 1st of November last year, my first big research project began with me as Chief Investigator, and I’d like to tell you all about it and my journey to get here! It’s called “CancerLearn” and aims to improve cancer diagnosis in people with learning difficulties.
There are around 1.5 million people with learning disabilities in the UK. The term ‘learning disabilities’ covers varying degrees of intellectual impairment, and diverse support needs, but is defined by a lifelong reduced intellectual ability and difficulty with everyday activities.
We know that People with learning disability experience health inequalities; the patient-related reasons for this are multifactorial and intersectional (complicated!), including severity of communication impairments, levels of regular contact with healthcare professionals, level of caregiver support, and other social factors influencing health.
Healthcare systems also affect outcomes for People with learning disability, due to e.g. lack of access, ableism and discrimination, unhelpful staff attitudes, lack of awareness or recognition of LD needs, and “diagnostic overshadowing” – where symptoms or disease features are mistakenly put down to the learning disability.
Spotting early signs of cancer can be very difficult, both for patients and for GPs, so how do people with learning difficulties fair in the cancer diagnostic pathway?
Not well (in general).
Over the last few years, I’ve led a work package in a programme called Spotting Cancer Among Comorbidities (SPOCC) that is exploring how patients’ pre-existing chronic health conditions impact diagnosing cancer. Using GP and hospital record data from 288,000 patients with cancer, we found that the more burden of illness people had across all their conditions the more likely they were to be diagnosed at an early stage, meaning treatment is more likely to be successful. When we looked at health conditions one by one, however, there were some the clearly imparted serious disadvantage in the cancer diagnostic process.
People with learning disabilities had the worst outcomes overall; they were 42% more likely to be diagnosed at a late stage, 2.6 times more likely to be diagnosed after being admitted to hospital as an emergency and 3.7 times more likely to die within 30 days of diagnosis.
I knew this issue was important to take forward; that we needed to dig into the factors that were leading to the poor outcomes and find innovative ways of reducing the inequalities. That would require more than the data-crunching we’d done so far – but as a data scientist and statistician, that’s kinda my thing!
So, joining the team of myself, Gary Abel and Bianca Wiering at Exeter, Geogia Black (Queen Mary University London) brought research experience of GP-patient communication and inequalities in cancer pathways using ethnographic methods, and Professor Katriina Whitaker (University of Surrey) and her team added experience of research with people with learning difficulties, particularly around cancer symptom awareness.
Together with Diana Frost, an expert by experience in cancer diagnosis, and Scott Watkin CBE, expert by experience in learning disabilities, as co-applicants and a group of 6-8 people with learning disabilities as a patient advisory group, we designed the CancerLearn project.
The aim of CancerLearn is to produce a comprehensive picture of what causes inequalities in cancer diagnostic outcomes for People with learning disability, what innovations exist to redress these in the symptomatic cancer pathway and whether these are amenable to scalable implementation.
We’ve operationalised this aim into sever research questions (RQs):
RQ1: What are the main personal, social and organisational factors that contribute to inequalities in cancer diagnostic outcomes for people with learning disability?
RQ2: What is the current evidence for interventions to support symptomatic cancer diagnostic pathways for People with learning disability?
RQ3: Where in the diagnostic process are avoidable delays occurring for People with learning disability?
RQ4: What features of cancer do People with learning disability tend to present with and are they reliably acted on with referrals and investigations?
RQ5: How are symptomatic cancer diagnostic pathways and innovations for People with learning disability currently experienced by patients and carers, healthcare staff, social care, system leaders and charities?
RQ6: How does local context affect implementation of innovations to redress inequalities in cancer diagnostic outcomes for People with learning disability?
RQ7: What are the acceptable and feasible possibilities for tailoring existing innovations or designing new innovations to redress inequalities in symptomatic cancer diagnostic pathways for People with learning disability at scale?
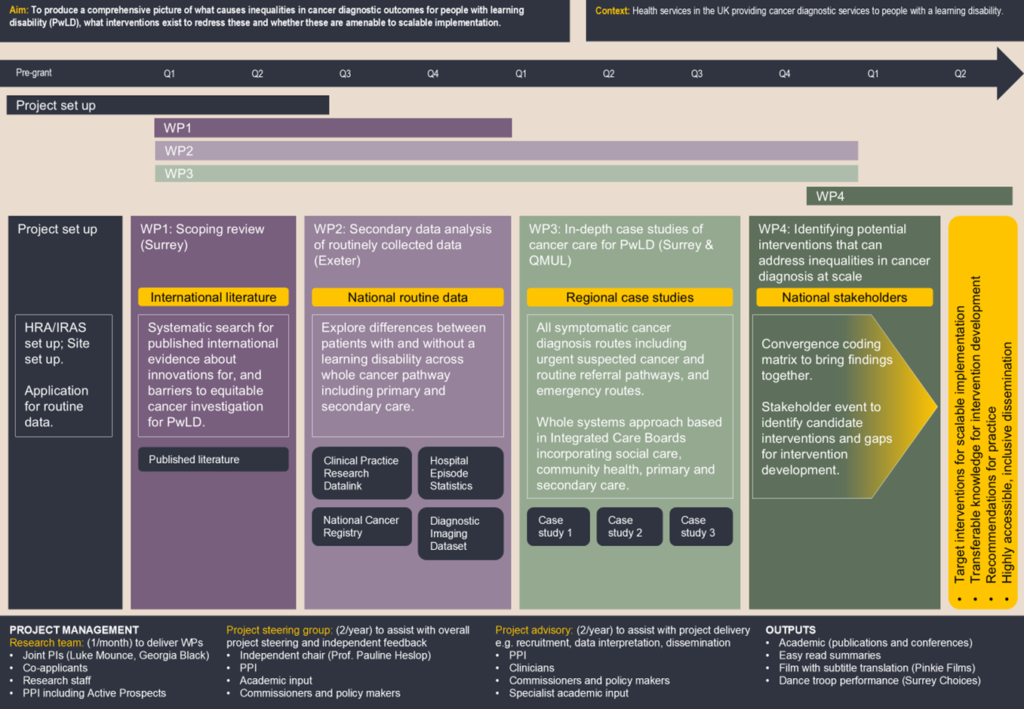
To answer these questions, we have 4 interconnected work packages (WPs), using a mixed-methods approach, running over 30 months. These are illustrated in the flow diagram below.
At the end of the project, we will hold a day-long event to share the study findings with stakeholders. To make the study findings as accessible as possible, we will create short films and easy-read summaries, and even have costed for an interpretive dance performance! Key stakeholder groups that we will engage include People with learning disability, support groups, Cancer Alliances, Integrated Care Systems, health and social care staff, and academics. We will leverage national charity and healthcare networks to reach patients, NHS organisations, and social care providers. We aim to integrate our findings into healthcare practices and guidelines around improving healthcare for people with learning disabilities, maximising impact on patient outcomes and healthcare delivery.
To support the work and help keep the project on track to meet its milestones, we have two advisory groups and steering committee. Our patient advisory group is being co-ordinated by Active Prospects (https://activeprospects.org.uk/), an advocacy charity for people with learning disabilities. Our clinical advisory group includes GPs, secondary care consultants, learning disability nurses, and Rachel Snow-Miller, head of the LeDaR programme (https://bnssghealthiertogether.org.uk/our-work/ledar-programme/).
CancerLearn will be unique in examining the journeys and experiences of People with learning disability through the cancer diagnosis process and we believe it will have international relevance. We anticipate that this work will identify targets for intervention and examples of innovation which may be amenable to implementation at scale, to ultimately improve cancer diagnosis for People with learning disability – with findings highly likely to be applicable to a much broader health context. We hope to better understand the need for, and required facets of, any future innovations. Development, and evaluation of such innovations will form the basis of future funding applications.