Exeter Collaboration for Academic Primary Care (APEx) Blog
Exeter Collaboration for Academic Primary Care (APEx) Blog
Posted by ma403
15 April 2025Associate Professor Christopher Clark
We know how to lower blood pressure with drugs, and quite a lot about how health professionals can help people to treat their hypertension. (1) Evidence to support these interventions is well summarised in various international hypertension guidelines, which also reinforce lifestyle changes to lower blood pressure and reduce cardiovascular risk. (2, 3) Such changes include salt restriction, weight loss, increased activity, smoking cessation and moderation of alcohol consumption. In general, however, guidelines lack practical guidance for either patients or professionals as to how to achieve such changes.
So, what about stress and relaxation? Stress and anxiety are thought of as risk factors for hypertension and cardiovascular events. (3) It is unclear whether this is a direct association, or rather that increased stress is linked to unhealthy behaviours such as greater use of alcohol, smoking or comfort eating. Interventions to relieve stress such as yoga, meditation or breathing control are still suggested (albeit with low certainty) in the current European hypertension guidelines. (3) However, advice to consider relaxation within a holistic approach to blood pressure lowering was dropped from the National Institute of Health and Care Excellence (NICE) guidelines for hypertension in 2019, due to the absence of outcome data to support the recommendation. (2)
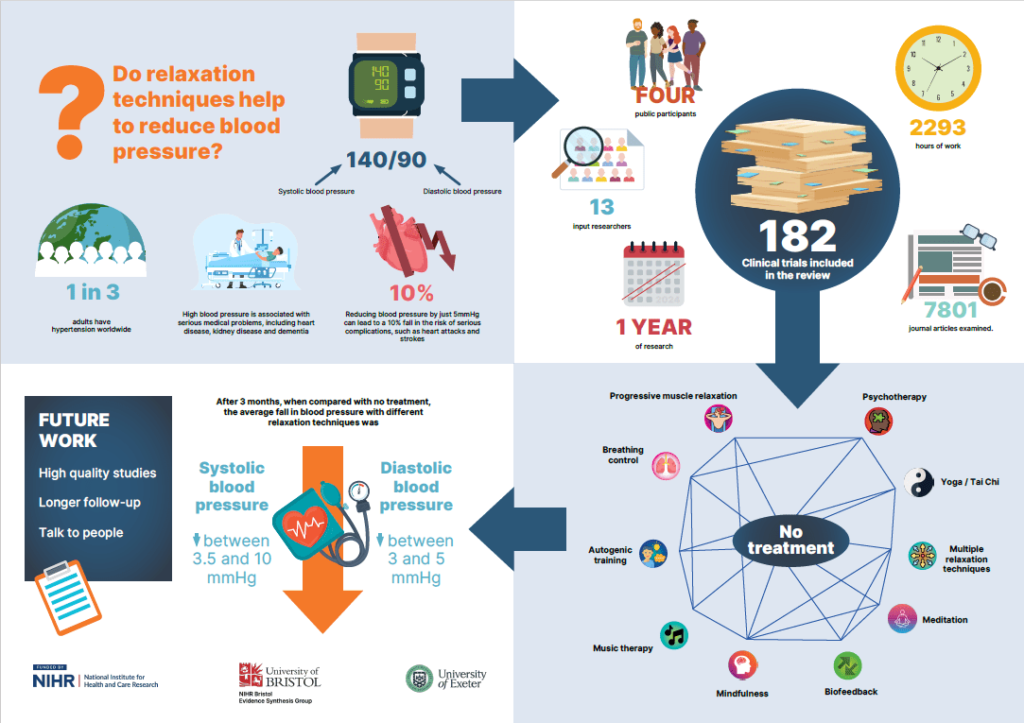
In a new systematic review and network meta-analysis, led by colleagues in the NIHR Bristol Evidence Synthesis Group, and published in BMJ Medicine[CC1] , we have now synthesised the evidence for stress management and relaxation interventions in managing high blood pressure. (4)
Our review included 182 studies (166 for hypertension and 16 for prehypertension). Results from a random effects network meta-analysis showed that, at short term follow-up (≤3 months), most relaxation interventions appeared to have a beneficial effect on systolic and diastolic blood pressure for individuals with hypertension.
Moderate reductions in systolic blood pressure ranging from −7 mmHg to −10 mmHg were found with breathing control meditation, meditative movement (including Tai Chi and yoga), mindfulness, music listening, progressive muscle relaxation and psychotherapy, Reductions were also seen in diastolic blood pressure.
Few studies conducted follow-up for more than three months, but effects on blood pressure seemed to lessen over time. Only limited data were available for prehypertension. The certainty of the evidence was judged to be very low due to the risk of bias in the primary studies, potential publication bias, and imprecision in the effect estimates.
So, can we recommend yoga, Tai Chi and other popular stress relaxation techniques to our hypertensive patients? As we discovered, there is evidence for a blood pressure lowering effect but we found no data on outcomes or on cost-effectiveness; a call for higher quality and larger studies of relaxation studies is one of the research recommendations in the current NICE guideline. (2)
In a separate review recently published in the British Journal of General Practice[CC2] , our group summarised the blood pressure lowering effects of interventions delivered as group activities, including relaxation therapies and exercises such as Tai Chi and yoga. (5) Subgroup reporting was limited due to small numbers of studies but, overall, when compared to usual care alone, systolic blood pressure was reduced on average by 7 mmHg following exercise interventions and 4 mmHg following psychotherapeutic interventions. These findings were similarly limited due to short duration of studies and high risk of bias.
In summary then, we have some short-term evidence for lowering blood pressure through relaxation techniques delivered either individually or within a group setting. Currently, little structured lifestyle information or self-help guidance is offered to people with newly diagnosed hypertension. We need future high quality studies, adequately powered to assess outcomes and including health economic assessments, to establish whether such a service could be recommended to the NHS in the future.
News release:
Relaxation techniques may help lower high blood pressure—at least in the short term – News
References
1. Clark C, Smith L, Cloutier L, Konya J, Todkar S, McDonagh S, et al.Interventions to improve control of hypertension; what works (and what doesn’t): systematic review and meta-regression. Can J Cardiol. 2018;34(10):S130-S1.
2. National Institute for Health and Care Excellence. Hypertension in adults: diagnosis and management (NG 136); Last updated: 21st November 2023. 28/8/19 ed. London; 2019.
3. Mancia G, Kreutz R, Brunström M, Burnier M, Grassi G, Januszewicz A, et al.2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension Endorsed by the European Renal Association (ERA) and the International Society of Hypertension (ISH). J Hypertens. 2023:10.1097/HJH.0000000000003480.
4. Webster KE, Halicka M, Bowater RJ, Parkhouse T, Stanescu D, Clark CE, et al.Effectiveness of stress management and relaxation interventions for management of hypertension and prehypertension: systematic review and network meta-analysis. BMJ Medicine. 2025;4(1):e001098.
5. McDonagh ST, Reburn C, Smith JR, Clark CE. Group-delivered interventions for lowering blood pressure in hypertension: a systematic review and meta-analysis. British Journal of General Practice. 2025;75(753):e266-e76.
[CC1]Effectiveness of stress management and relaxation interventions for management of hypertension and prehypertension: systematic review and network meta-analysis | BMJ Medicine
[CC2]Group-delivered interventions for lowering blood pressure in hypertension: a systematic review and meta-analysis | British Journal of General Practice