Models of Care for people living with Multiple Long-Term Conditions
Research priority setting
Models of Care for people living with Multiple Long-Term Conditions
Research priority setting
Posted by Jo Butterworth
3 September 2025Dorian Poulton, NIHR undergraduate intern with the cross-NIHR-collaboration (CNC) for Multiple Long-Term Conditions (MLTC) – Models of Care workstream, Summer 2025
Developing effective models of care for MLTC is a significant concern for patients, their carers, clinicians and those involved in managing the health system. This is because the current model of care often focuses on single diseases or organs and struggles to support patients who have multiple conditions due in part to the interactions between different conditions and the effects treatment for one condition can have on a patient’s other diseases.
This project aims to review previous research done on models of care for multiple long-term conditions and identify the research priorities of patients living with MLTC, carers, clinicians, policymakers, and care commissioners. The first part of the study involved a scoping review of research into models of care for MLTC to identify the research priorities of patients, carers clinicians, policymakers, and care commissioners as well as to identify missing perspectives in the existing literature.The second part of the project will be a James Lind Alliance (JLA) priority-setting partnership. This involves engaging external groups to support the recruitment of patients, carers, clinicians, policymakers, and care commissioners to complete two rounds of a survey to facilitate research prioritization. The final step of the JLA is a workshop in which representatives from the various participant groups decide the final, top 10 research priorities.
I served as an undergraduate intern for the project, spending five weeks at the Exeter Collaboration for Academic Primary Care (APEx) during August 2025. My placement covered many aspects of the project and I met with members of the CNC for MLTC Models of Care workstream. I was able to assist with the full-text review of literature for the scoping review and assist with the piloting of the review’s data extraction template. I also produced the initial version of the JLA protocol for the project and completed an equality impact assessment (EqIA) of the initial protocol.
To support the EqIA, I led a meeting with the project’s patient-public involvement (PPI) panel. The PPI meeting was split into two parts, with the initial part exploring potential strategies for the JLA. The PPI panel proposed a range of possibilities, including conducting outreach through online forums specific to a protected characteristic, such as recruiting via online parental support forums to try and recruit pregnant and postnatal people, utilizing community hubs as sites of in-person recruitment and attempting to encourage participants to disseminate the survey throughout their own social networks to broaden its reach.
Prior to the meeting, PPI panel members were asked to produce a sketch showing the journey (either their own or that of the person they care for) to formal diagnosis of their condition and support. During the second part of the meeting, a selection of these sketches were discussed with the whole PPI panel.
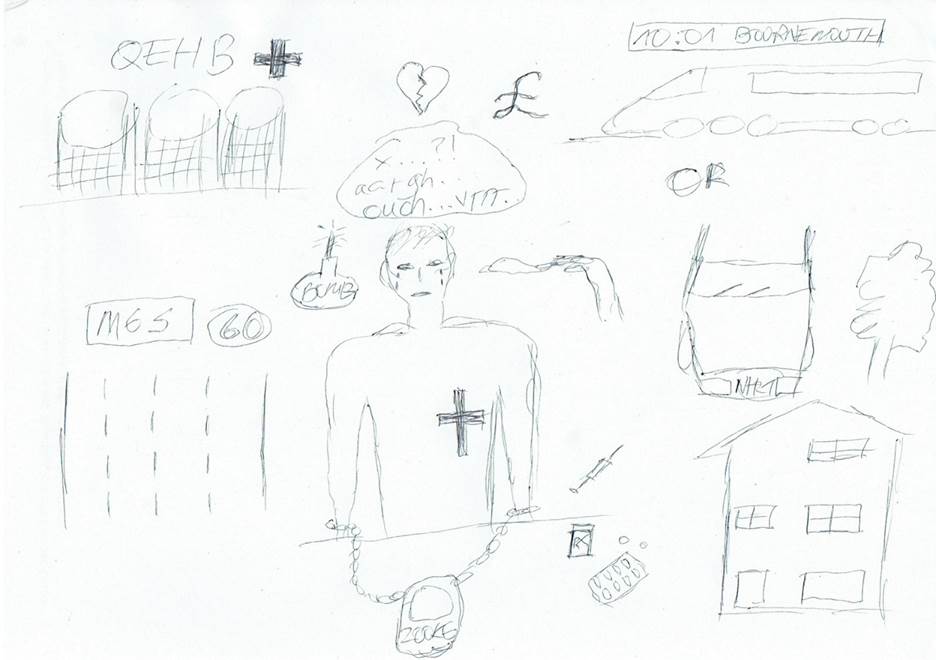
PPI panel member Kamil produced this sketch, highlighting the logistical, financial and emotional burdens that are placed upon patients navigating the healthcare system.
These sketches, and the conversations they sparked during the PPI panel meeting, highlighted the need for health research projects to find alternatives to current inclusion criteria, which typically rely on formal medical diagnoses, and instead consider identifying or developing alternative measures to evaluate the potential MLTC of research:
not all people providing care identify with the term ‘carer’
As a result of these failures, these patients are often unable to participate in health research – as they lack the required diagnosis – and even when they do meet the inclusion criteria many of them are distrustful of clinicians and healthcare research due to their prior aversive experiences. The PPI panel also highlighted that not all people providing care identify with the term carer, due in part to differences in cultural expectations around caregiving, particularly for family members, viewing care as a shared responsibility of the whole community and/or carers engaging in deeply reciprocal models of care in which labour and resources are shared across a network of people.
To support the development of the protocol for the JLA, I developed an Equality Impact Assessment (EqIA) to ensure that the planned study was accessible, unlikely to harm marginalized communities or exclude potential participants due to their protected characteristics. The EqIA also helped identify potential means of addressing identified equality issues in the JLA process.
I began with a review of the JLA protocol and previous research into health inequalities, access to care for marginalized communities, and common barriers to health research participation. This review helped identify groups at risk of being harmed or excluded from the EqIA, those most likely to benefit, and potential solutions to inequalities in the study. These included
These changes should help ensure that potential participants are not excluded due to unsuitable recruitment methods, inaccessible survey materials, being misgendered or faced with microaggressions in the survey and that communities which have different cultural expectations around care are able to participate.
My placement has been a most useful experience. Over the course of the internship, I was able to critically engage with research surrounding models of care for MLTC, health policy and the way care is currently organized for patients with complex conditions, which has significantly strengthened my knowledge in this area. Running a PPI panel meeting was a particular highlight of my internship. It provided significantly more nuance to the EqIA and helped inform potential recruitment strategies, such as targeting social clubs and community centres for in-person recruitment. The PPI meeting also allowed me to further develop my confidence in collaborating with non-academic contributors and in utilizing creative methods to examine deeply emotional topics.