Haemochromatosis: genetic iron overload disease
Summary for patients
Haemochromatosis: genetic iron overload disease
Summary for patients
Sex
The accumulation of iron in the body over time can cause some haemochromatosis patients to develop complications that impact vital organs and joints. Such complications typically present themselves earlier in males compared to females [1], thought to be as a result of iron lost through the menstrual cycle in women. However, symptoms may begin to emerge in females after menopause.

Age
Because iron accumulation in the body takes a long time to build up and start damaging the organs and joints to a detectable level, signs and symptoms of the disease usually present during middle age (40s and 50s years), with males typically developing symptoms earlier than females. Although, signs and symptoms can still present themselves for the first time in older individuals (>60 years). [1]

Alcohol
Alcohol intake is a well-known risk factor that increases the risk of haemochromatosis, whilst also enhancing the clinical expression of haemochromatosis-related symptoms [2]. Alcohol consumption has been shown to increase the amount of iron in the body, especially regular excessive alcohol consumption. Being a carrier of a high-risk haemochromatosis genotype, such as two copies of the C282Y variant, plus the consumption of alcohol, can significantly increase the risk of haemochromatosis-related complications, such as liver disease and liver cancer.

Diet
Excessive accumulation of iron in the body is the main cause of complications in haemochromatosis. However, it is unclear if controlling dietary iron intake will affect the severity of haemochromatosis symptoms [3]. Nonetheless, it is important to avoid any iron-based supplements. Please discuss any changes to your diet with a health professional for personalised advice and guidance.
Obesity
The accumulation of excessive fat in the liver, otherwise known as non-alcoholic fatty liver disease (NAFLD), can contribute to raised iron measures in individuals with hemochromatosis. The combination of excess fat in the liver among haemochromatosis patients may exacerbate damage to the liver. Our research found that a high waist-to-hip ratio, a marker of central adiposity, is associated with an increased risk of liver complications in both C282Y homozygous males and females [4].

Other genetic variants
There are many common genetic variants that each alter iron levels a little, but which together can cause people with the main HFE variants to seriously overload iron [5]. Also, there are many small effect variants for liver disease, arthritis and diabetes, which can add to a persons risk of getting these diseases with or without HFE variants.
Genetic background
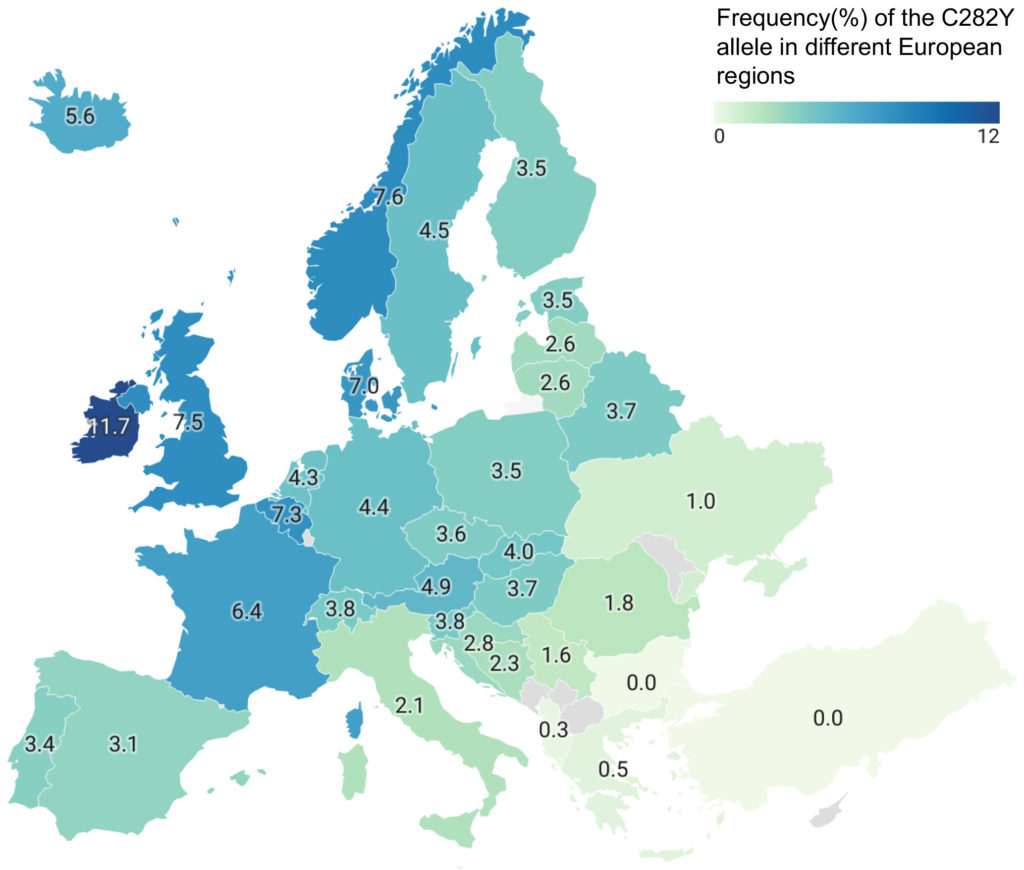
The HFE genetic variants are most common in individuals of European genetic ancestry [6], especially Northern Europe (indeed, the disease is sometimes known as the “Celtic curse”). The figure below shows the C282Y allele frequency (% occurrence) varying over Europe. We therefore restricted our analysis to participants of European genetic ancestry, thus our results do not necessarily reflect risk of haemochromatosis based on HFE genotype for other genetic background.