Haemochromatosis: genetic iron overload disease
Summary for patients
Haemochromatosis: genetic iron overload disease
Summary for patients
You have one of each copy of the HFE C282Y and H63D genetic variants.
* Estimates are from our community sample of UK Biobank European descent individuals [1]. People tested because of a health problem or with high iron levels may have different risk. See below Technical Details section for more information, and the Other Risk Factors page for risk modifiers. Page updated 12th February 2024.
Males are known to have higher risk of iron overload disease compared to females.
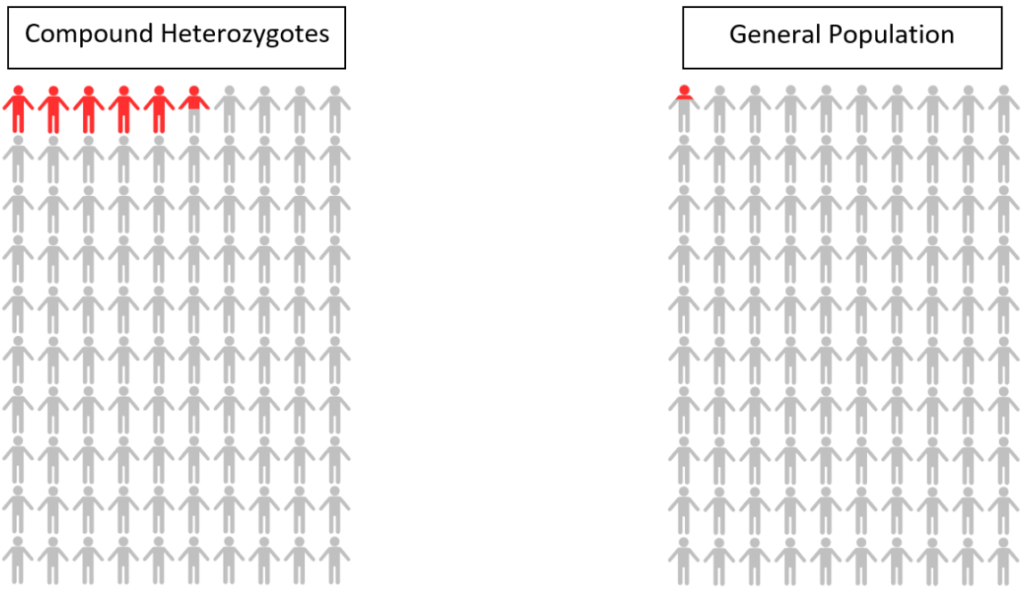
Haemochromatosis – We estimated that 5.4% of UK Biobank males with one of each copy of HFE C282Y and H63D would be diagnosed with haemochromatosis by age 80, compared to 0.2% of individuals with no faulty HFE genes.
Risk of disease/mortality – In our study of mortality and disease risk to age 80 in UK Biobank, males with one of each copy of the HFE C282Y and H63D genetic variants did not have increased risk of death or liver complications (including liver disease and liver cancer).
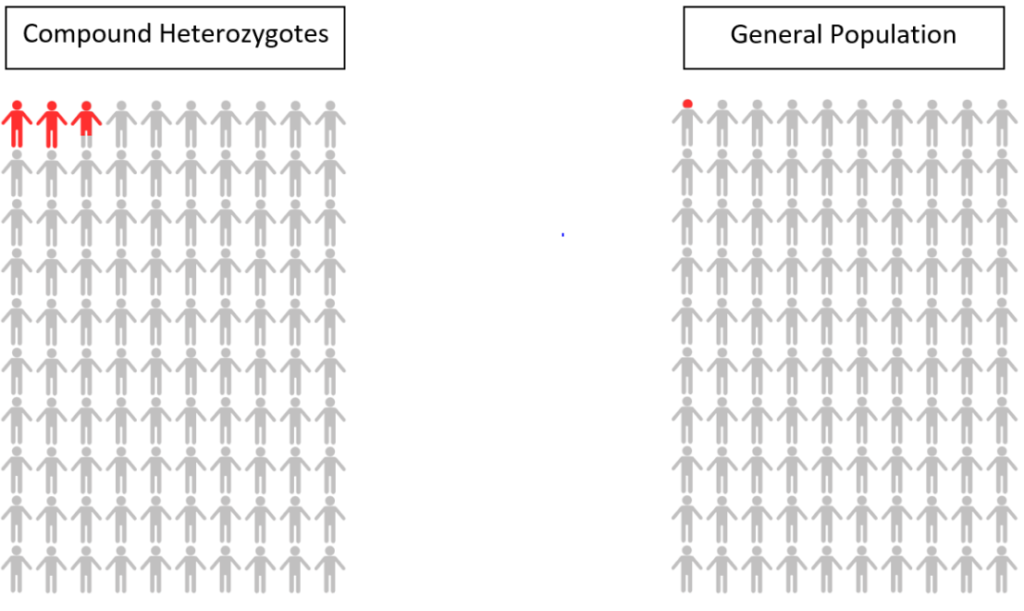
Haemochromatosis – We estimated that 2.7% of UK Biobank females with one of each copy of HFE C282Y and H63D would be diagnosed with haemochromatosis by age 80, compared to 0.1% of individuals with no faulty HFE genes.
Risk of disease/mortality – In our study of mortality and disease risk to age 80 in UK Biobank, females with one of each copy of the HFE C282Y and H63D genetic variants did not have increased risk of death or liver complications (including liver disease and liver cancer).
Because you have one copy of each of the HFE C282Y and H63D gene variants, it is unlikely to be haemochromatosis. If you experience symptoms they are not likely due to haemochromatosis, but you should contact your GP if they persist or become more severe. See below for guidance:
The UK NHS website for haemochromatosis (link) says to speak to your GP about getting a test if:
1. See below effect estimates for disease and mortality for male and female compound heterozygotes, note that all results are statistically non-significant after applying calculations to adjust for multiple testing:
2. Genetic differences among different populations can influence the risk of disease prevalence and rates of mortality. Therefore, the generalisability of our study findings may be limited to individuals of European descent.
3. Early follow-up years are liable to be impacted by healthy volunteer bias in the UK Biobank. However, the present study’s findings reported incident outcomes with sufficient follow-up time (median of 13.3 years), thus, limiting the influence of a healthy volunteer bias.
4. The current study does not take into account other genotypes that are known to influence iron metabolism. Therefore, the potential implication of such modifiable effects on iron could have affected any associated risks of disease or mortality. However, further research is required to determine the extent of such effects.
5. Adjusting for multiple testing refers to a statistical procedure used to control the overall false positive rate or Type I error rate when conducting multiple statistical tests.
[1] Mitchell R Lucas, Janice L Atkins, Luke C Pilling, Jeremy D Shearman, David Melzer. HFE genotypes, haemochromatosis diagnosis and clinical outcomes at age 80: a prospective cohort study in the UK Biobank. BMJ Open. 2024; doi:10.1136/bmjopen-2023-081926
[2] UK NHS Haemochromatosis overview – https://www.nhs.uk/conditions/haemochromatosis/